Rudoph and Link in 2002 found that feeding disorders occur in 25-35% of developmentally normal children and 40-70% of children with developmental disabilities and/or chronic medical conditions.
Looking at this study, it is obvious that feeding disorders are more common that we think. Here are some questions we get asked frequently:
 Why does my child take a long time to have food?
Why does my child take a long time to have food?
Why does she/he not prefer all foods?
Why are they just swallowing everything in their mouth without chewing?
Why are mealtimes becoming so difficult?
The idea behind this blog is to help the readers understand and relate to the oral sensory and oral motor challenges that children might face. This is turn would help you all get a better idea about the child’s needs and what would help them with healthy growth and development.
Feeding a child is not only critical for survival; it’s also an integral part of our social experience. A child who can’t eat or won’t eat can have a serious impact on the entire family’s quality of life.
Feeding issues typically fall into one of two categories (or a combination of the two): oral motor issues and/or sensory issues.
ORAL MOTOR DIFFICULTIES:
 The oral-motor aspect of eating involves how the mouth muscles function: how strong the muscles are, how well they coordinate the range of motion and how far they can move as they manipulate food in the mouth. Although eating is very simple/automatic for most of us, it’s actually very complex. The jaw moves in a rotary motion to chew and adequately break down the food. At the same time, the tongue manipulates food from side to side and up and down to assist in breaking down the food, ultimately forming the food particles into a bolus in preparation for the swallow. It’s complicated! It requires tongue lateralization, tongue elevation, jaw strength, rhythmic chewing, coordination, etc.
The oral-motor aspect of eating involves how the mouth muscles function: how strong the muscles are, how well they coordinate the range of motion and how far they can move as they manipulate food in the mouth. Although eating is very simple/automatic for most of us, it’s actually very complex. The jaw moves in a rotary motion to chew and adequately break down the food. At the same time, the tongue manipulates food from side to side and up and down to assist in breaking down the food, ultimately forming the food particles into a bolus in preparation for the swallow. It’s complicated! It requires tongue lateralization, tongue elevation, jaw strength, rhythmic chewing, coordination, etc.
ORAL SENSORY DIFFICULTIES:
The oral-sensory is mainly related to the tissues in the mouth, i.e., perceiving sensory information such as the taste, temperature and texture of food. Sensory food aversions can be present in one of two ways (or again, sometimes in combination):
-
Hypo-sensitivities,
 meaning little to absence of oral awareness, where we could see behaviours such as mouth stuffing (also known as food pocketing) or children loving to eat food through the day or children having leftover food particles in their mouth or drooling. All these behaviours noticed are mainly because the child cannot feel enough in their mouth. So, if the child cannot feel food/food particles in the mouth, he/she won’t know to retrieve and swallow them.
meaning little to absence of oral awareness, where we could see behaviours such as mouth stuffing (also known as food pocketing) or children loving to eat food through the day or children having leftover food particles in their mouth or drooling. All these behaviours noticed are mainly because the child cannot feel enough in their mouth. So, if the child cannot feel food/food particles in the mouth, he/she won’t know to retrieve and swallow them. -
Hyper-sensitivities,
 meaning too much oral awareness. In this case, the child may gag or vomit, spit the food out, turn away from the food, resist by crying/kicking/screaming, present with a range of behavioral issues, etc.
meaning too much oral awareness. In this case, the child may gag or vomit, spit the food out, turn away from the food, resist by crying/kicking/screaming, present with a range of behavioral issues, etc.
SYMPTOMS OF ORAL-MOTOR AND ORAL-SENSORY PROBLEMS:
|
Symptoms of a motor problem could include:
|
Symptoms of a sensory problem could include:
|
HOW DO SENSORY -MOTOR SYSTEMS COME TOGETHER DURING FEEDING?
The sensory and motor systems function as a feedback loop. Sensory input impacts motor skills and movement impacts sensory perception. If a child has difficulty differentiating taste, texture, temperature, or locations of food in the mouth it may be difficult to handle food safely (Bahr, 2001). Holding food in the mouth for long periods of time, swallowing foods that are not adequately masticated (chewed), eating non-food items, etc. may result in gagging, choking, and vomiting. Food refusal and self-limited diets are often the result of compromised oral sensory-motor skills and negative experiences which result in behavioral responses (Overland & Merkel-Walsh, 2013).
For example, a typically developing toddler may react surprised, interested, or slightly dismayed when introduced to a new food taste. In fact, a toddler with feeding issues may become hysterical, turn red, and start gagging.
ASSESSING FEEDING ISSUES
When a child with feeding problem is referred to a Speech-Language Pathologist (SLP) for self-limited diet, a comprehensive feeding assessment is required, including a review of the child’s medical status; gross, fine, and oral-motor development; nutritional status; and sensory processing (Arvedson & Brodsky, 2001). Since the sensory and motor systems cannot be separated (Overland & Merkel-Walsh, 2013), it is very important to task analyze the child’s motor skills and determine how they relate to feeding, before assuming that a self-limited diet is purely behavioral (Overland, 2010; Merkel-Walsh, 2012).
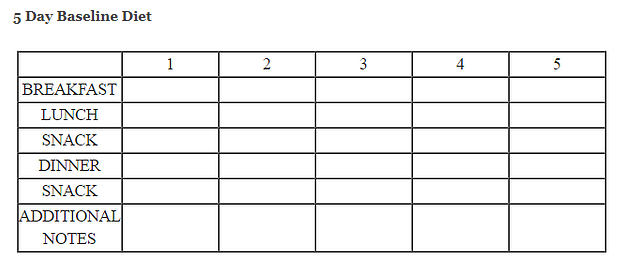
In order to understand a child’s diet profile, it is important to collect the necessary data and analyze that data in conjunction with information collected on the child’s oral sensory-motor skill development (Overland & Merkel-Walsh, 2013). To meticulously understand a child’s taste, temperature and texture preferences, a diet report on five days would be helpful. Filling out a form reporting all foods consumed over five days, including brands of foods, amount consumed, and the utensils that were used. This helps the therapist establish a “home base” which is a profile of taste, texture, and temperature in a child’s diet. Diet shaping starts with a child’s existing profile and slowly expands taste and texture. The therapist must look at the underlying oral sensory-motor skills to support safe, effective nutritive feeding.
MANAGING FEEDING ISSUES
Altering the child’s position significantly improves oral motor and swallowing function. Optimal positioning during feeding can
-
-
Support the child’s breathing (Massery,2012)
-
Allow the child to focus energy and attention on feeding rather than maintaining postural stability
-
Optimizes the child’s oral motor coordination, making chewing and swallowing easier (Redstone & West, 2004)
-
Promote digestive system efficiency
-
Often when we work with a child with feeding issues, it is tempting to look at the jaw, tongue and the lips and forget about posture. Thus, we need to decide on the seating arrangement that can give provide adequate pelvic stability which will support trunk control. This will in turn influence head control, jaw stability and oral motor control (tongue control and lip closure).
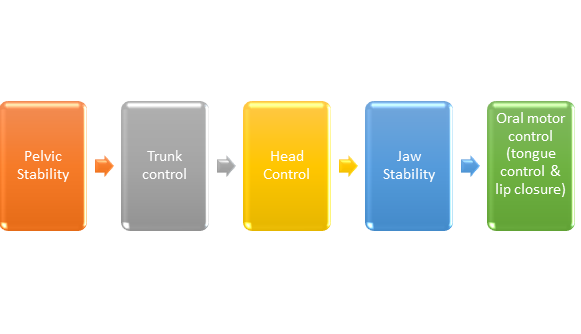
Adapted from Redstone & West (2004)
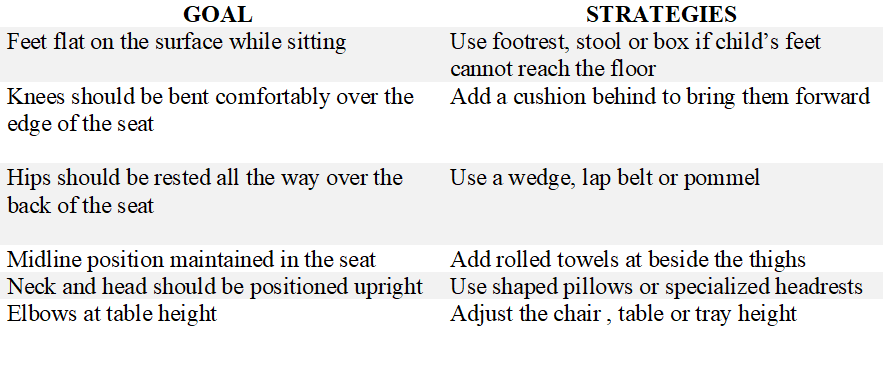
While deciding on the positioning, the following goals and arrangements need to be kept in mind.
After taking care of the right positioning, a speech pathologist can lead him or her through exercises that strengthen the mouth muscles and build proper feeding techniques. On the other hand, if a child is facing a sensory problem, the SLP/OT may recommend desensitization therapy (repeated exposure to problematic foods or textures) or may suggest modifying the child’s mode of feeding (for example, changing the type of bottle, cup or straw) until the child’s feeding abilities get improved. Playing with food is also a fantastic way of exposing children to food without the demand of “eating” it. As they are exposed to the food through play, they get used to the sight, smell and feel of the food on their hands. This would also help in the desensitization process, thus allowing more acceptance of food gradually into their mouth.
Hyposensitive children may need extra sensory information, such as extra flavoring, to recognize the presence of food. If there’s a behavioral component to your child’s feeding issue, the Psychologist helps in identifying the right kind of reinforcements, carefully deciding on the food choices and textures which can go a long way with treating feeding issues. Whatever approach we take, our goal is to make sure your child can eat safely and efficiently.
To know more about the structured treatment program we follow at PlayStreet, please do take a read through our article on Oral Placement Therapy (What is oral placement therapy?), which is a structured program that helps normalize oral muscle tone, create appropriate oral motor movements and improve feeding and speech skills.
To know more about importance of muscle tone in feeding, please have a read through https://www.playstreet.in/2021/01/18/oral-muscle-tone-in-speech-and-feeding/
REFERENCES:
-
https://www.asha.org/practice-portal/clinical-topics/pediatric- dysphagia/#collapse_2
-
https://www.saera.eu/en/2019/02/14/speech-therapy-feeding-issues/
-
https://journals.lww.com/jpgn/Fulltext/2016/09000/Oral_Motor_Impairment_i n_Children_With_Feeding.26.aspx
-
https://talktools.com/pages/feeding-therapy-a-sensory-motor-approach
-
https://sltforkids.co.uk/feeding-clinic/problems-we-help/sensory-based- feeding-difficulties/
-
https://www.arktherapeutic.com/blog/food-refusal-is-it-oral-motor-or-sensory-related/
-
https://ctspediatrics.com/treatment-areas/occupational-therapy/behavioral-sensory-feeding/
-
Carruth B, Skinner J. Feeding behaviors and other motor development in healthy children (2–24 months). Journal of the American College of Nutrition (2002) 21(2)
-
Gisel, E. G. Oral-motor skills following sensorimotor intervention in the moderately eating- impaired child with cerebral palsy. Dysphagia, 9, (1994).
-
Overland, L. A sensory motor approach to feeding. Professional lecture for Innovative Therapists International, Charleston, SC. (2010, June).
-
Rosenfeld-Johnson, S. Oral placement therapy for speech clarity and feeding. Tucson, AZ: Innovative Therapists International. (2009).
-
Palmer, S., & Horn, S. Feeding problems in children. In S. Palmer & S. Ekvall (Eds.), Pediatric Nutrition in Developmental Disorders. Springfield, IL: Charles C. Thomas.(1977).


0 Comments