
The term Dyspraxia was derived from the word ‘Praxis’ which means “the ability to perform intentional movements or simple gestures”, like playing with toys, using tools (including a pencil or a fork), building a structure (like a toy block tower or a house) or engaging in many occupations. (Ayres, Mailloux and Wendler, 1987).
Dyspraxia affects a significant number of children and adults. Barbara Lantin reports that “dyspraxia affects up to ten per cent [of the general population] and two per cent severely. As with dyslexia, 80 percent of those affected are boys” (Lantin, 1997).
Dyspraxia is a learning difference that affects how the mind processes actions, usually affecting coordination and movement.
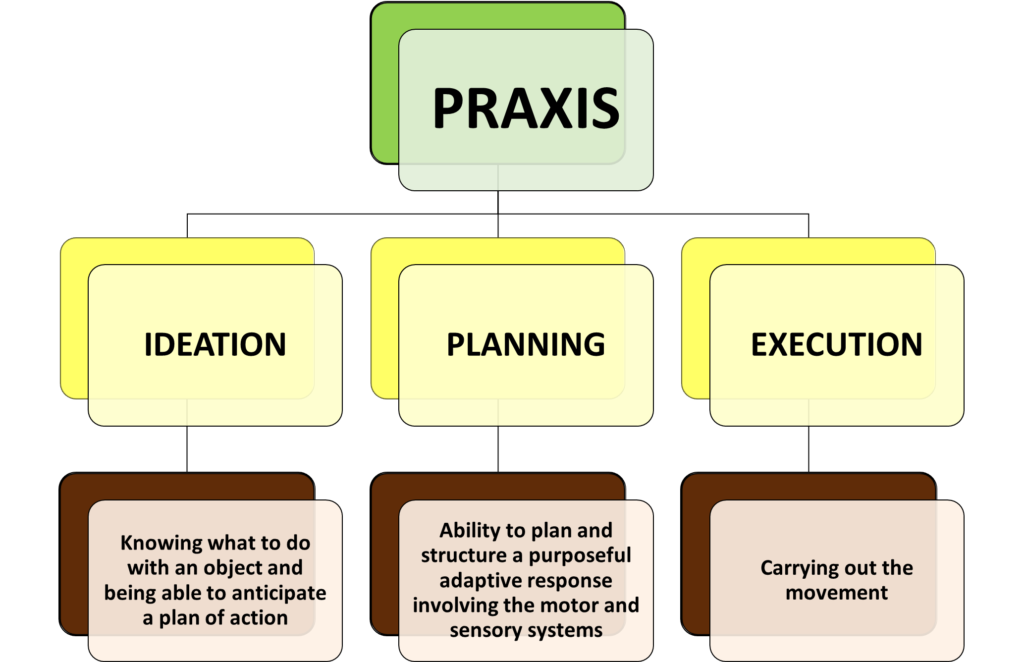
Dyspraxia is defined as difficulty in planning and carrying out skilled non-habitual motor acts in the correct sequence. It is not a primary problem in motor co-ordination (motor execution). Rather the problem is hypothesized to be due to difficulty in formulating the plan of action. (Ayres 1972a, 1979, 1985, 1989 in Fisher, Murray & Bundy, “Sensory Integration: Theory and Practice”, 1991, F.A. Davis Company, p. 141)
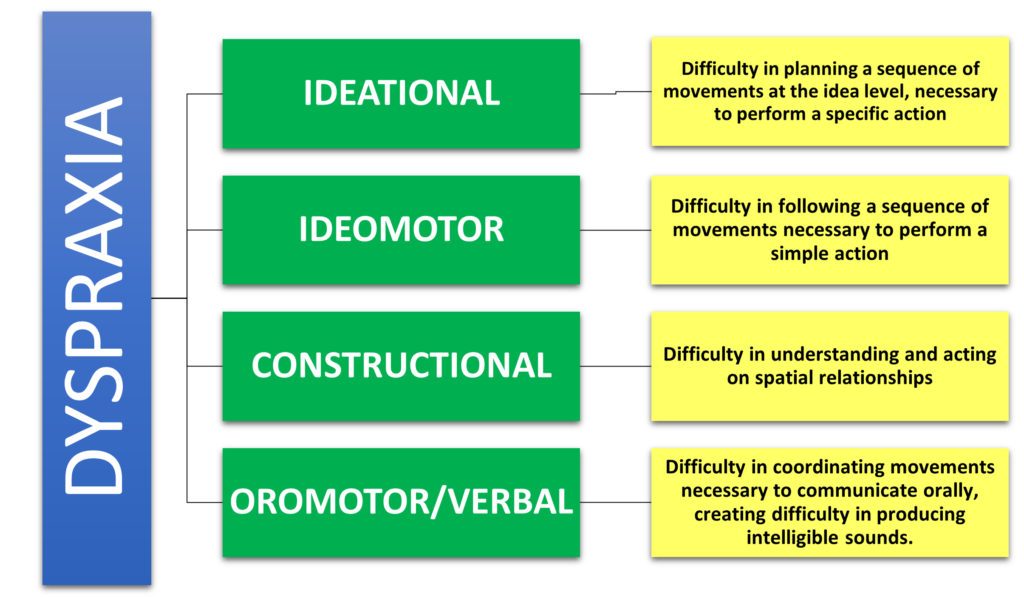
TYPES OF DYSPRAXIA:
SYMPTOMS OF DYSPRAXIA:
Developmental and Educational Symptoms

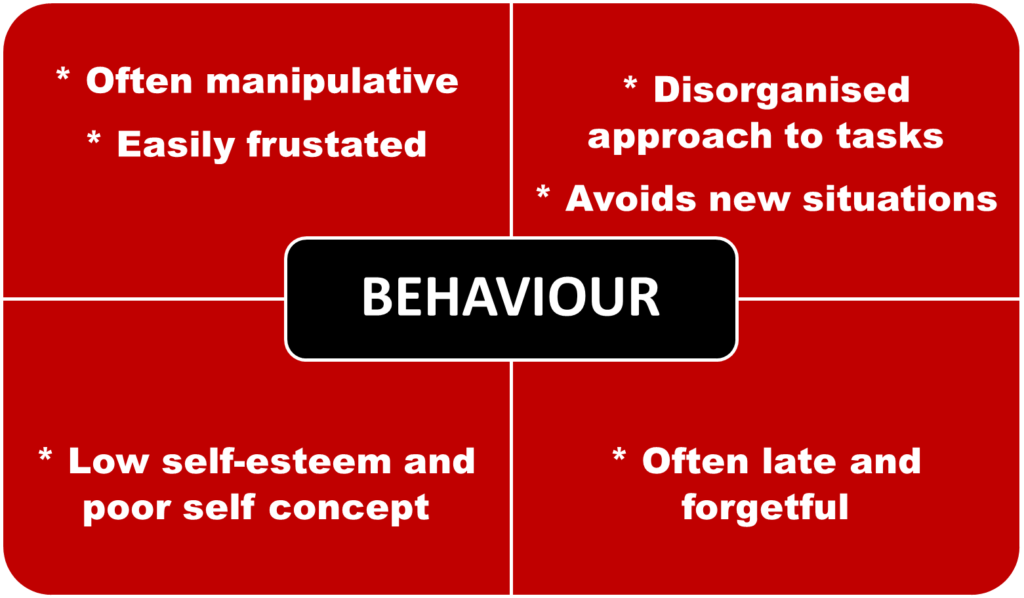
Behavioral characteristics
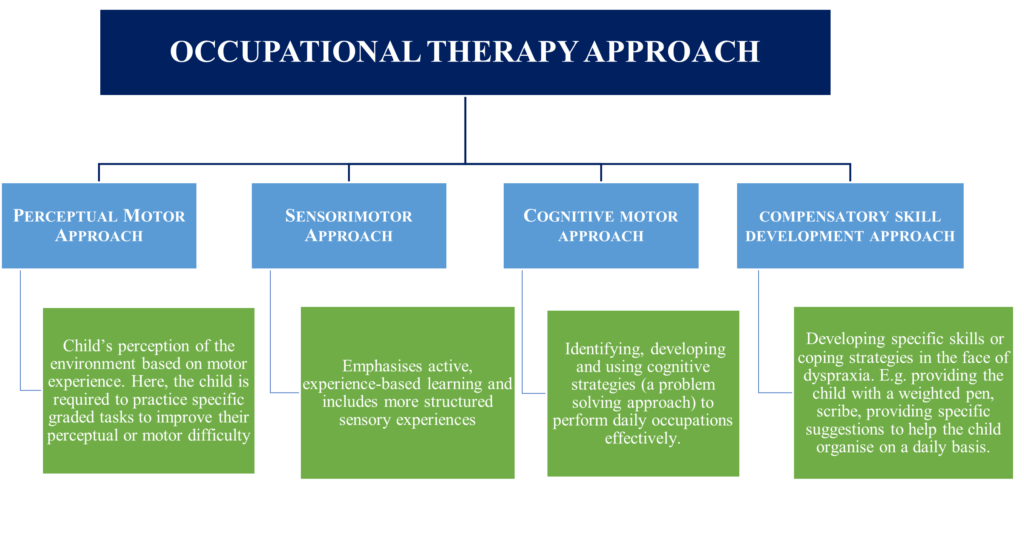
What do Occupational Therapists (OT) do?
-
Assessment:
-
Interview the mother/father/teacher and obtain information about the child’s current level of functioning and their early development.
-
Perform a classroom observation
-
Do non-standardized clinical observations of neuromotor behavior. For example, how does the child initiate active exploratory behavior, how does the child interact in class and other motor tasks.
-
Perform selected standardized assessments, e.g.: Sensory Integration and Praxis Tests (SIPT), Bruininks-Oseretsky Test of Motor Proficiency (BOT-MP), Movement Assessment Battery for Children, Developmental Test of Visual-Motor Integration, Test of Visual Perceptual Skills, Sensory Profile (Winnie Dunn), etc.
-
The OT will observe the way in which the child performs motor tasks, including quality of movement as well as the end skill. There is no ‘one’ test which can be used for assessment and information is looked at as a whole in order to draw up a pattern of difficulties and underlying problems. During an assessment, an occupational therapist will try to define more specifically the difficulties a child may present with. The child with dyspraxia usually achieves their motor milestones at appropriate ages but then has difficulty with more complex tasks. E.g., buttoning and fastening zippers.
Tips for Children with Dyspraxia:
-
Child can sit in the front of the class.
-
Predictable schedule and routine can be provided
-
Classroom/work area can be more organized
-
Instructions can be spoken slowly and repeated
-
Tasks that are completed correctly are acknowledged and praised.
-
Extra time is allowed for assignments.
-
Assistance is given for fine motor tasks. Stabilization of the hand is encouraged when writing.
-
Lined and graph paper can be provided as they really help the student organize spatially.
-
“Body breaks” should be allowed throughout the day.
-
Good posture is encouraged whenever possible.
-
Feedback is given as this helps manage the dyspraxia better.
Dyspraxia is not curable. However, children can learn new skills or refine the skills already present, or they can compensate for their difficulties. Students do not grow out of dyspraxia; they learn to accommodate their difficulties, and with early intervention, progress is accelerated. (Losse et al., 1991)
References and Useful Links:
-
Dyspraxia from an Occupational Therapy perspective: Natasha Patten BSc (Occupational Therapy)
-
Giving a Face to a Hidden Disorder: The Impact of Dyspraxia by Debi J. Stansell (https://files.eric.ed.gov/fulltext/EJ967468.pdf)
-
An Investigation of Dyspraxia: What We Know and Why the Research Is So Far Behind by Emily J. Meachon.
(https://www.researchgate.net/publication/321275661_An_Investigation_of_Dyspraxia_What_We_Know_and_Why_the_Research_Is_So_Far_Behind)
-
https://dyspraxiafoundation.org.uk/wp-content/uploads/2013/10/dyspraxia_and_Occupational_Therapy.pdf
-
https://dynamicoccupationaltherapy.com/ot-strategies-dyspraxic-students/
-
https://dyspraxiafoundation.org.uk/professionals/occupational-therapists/
-
https://www.griffinot.com/dyspraxia-symptoms-is-my-child-dyspraxic/



0 Comments